Re-thinking rehab for incontinence after prostate removal
This week is international men's health week, so it seemed fitting to write on a topic related to pelvic health in men. Interestingly enough, men are actually an underserved population when it comes to pelvic health. I know, shocking, but it's true. From a physical therapy standpoint there are way fewer clinicians who treat men than there are who specialize in women's health or prenatal/postpartum populations. In fact, I can't tell you the number of men I've seen in the clinic who tell me that they were turned away from multiple previous clinics or who saw another provider who clearly felt uncomfortable treating them.
For me, I knew when I started specializing in pelvic health over 10 years ago, that I wanted to treat ALL people. I never limited my training to vaginas, and I always tried to learn to serve everyone. When I opened Southern Pelvic Health last year, I wanted to build a clinic that could really serve ALL people. We treat anyone who comes in the door, and our clinicians and staff constantly strive to be educated to provide a safe and welcoming space for anyone we meet.
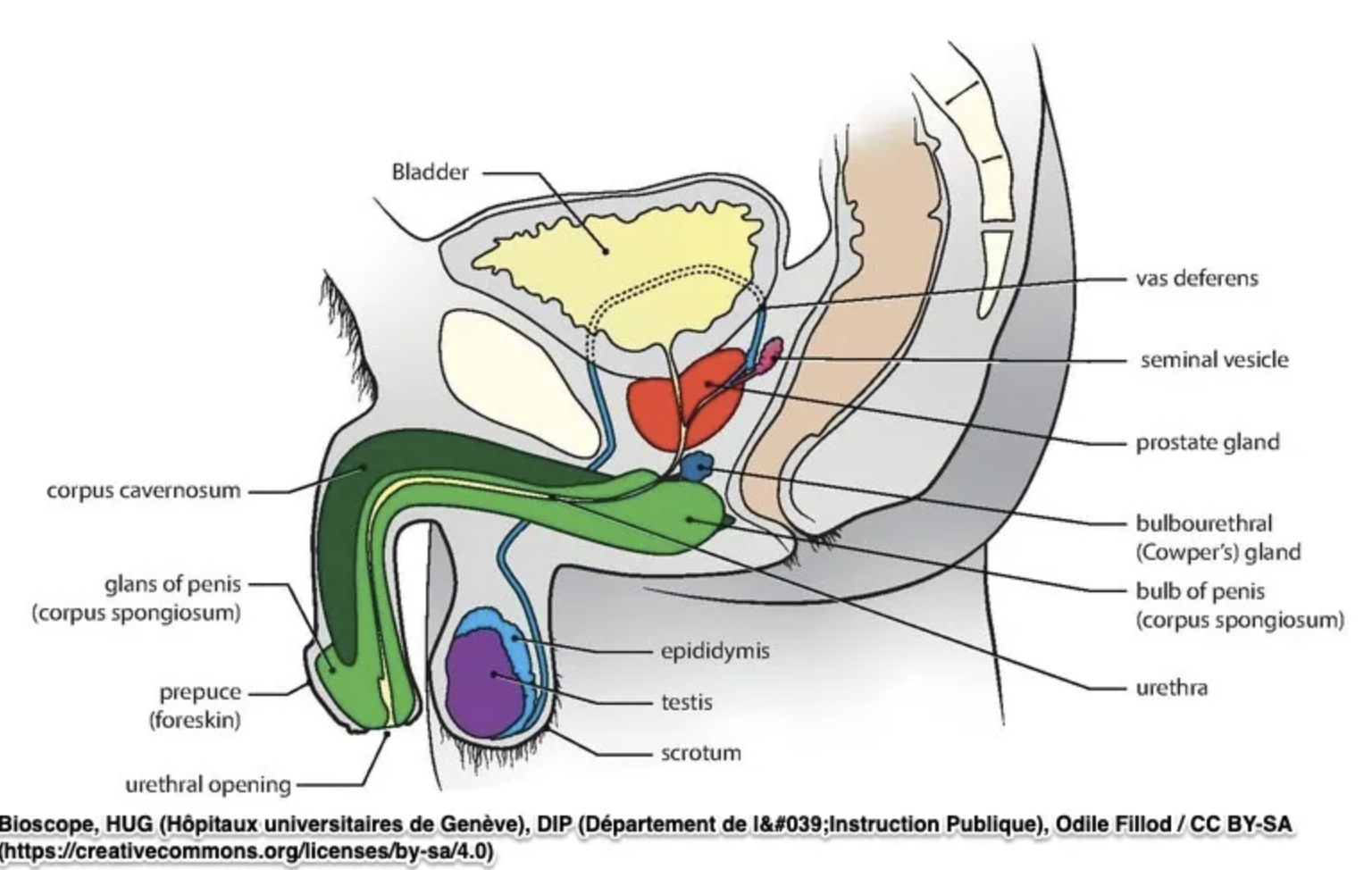
So, this brings us to Men's Health week! Today, I want to talk a little bit about rehabilitation after prostate removal surgery-- aka prostatectomy. Prostatectomies are most often performed when a person has prostate cancer, and involve removal of the prostate and the portion of the urethra that runs through the prostate. This is most often done robotically currently. Prostate removal surgeries can have some side effects, and one of the most annoying side effects is stress urinary incontinence. Sexual dysfunction is also a major side effect, and of note, these two side effects are ones that many express feeling unprepared for. These two can have a huge impact on quality of life of many individuals after surgery.
Why does incontinence happen after prostatectomy?
The prostate sits under the bladder, and thus, plays an important role in continence. There is an internal sphincter that is present at the level of the prostate right at the bladder neck, as well as an external urethral sphincter below the prostate, which is part of the pelvic floor muscles. When the prostate is removed, the support and sphincteric control at the bladder neck is impacted. Additionally, the external sphincter can be damaged with the surgery, and patients can also have damage to neurovascular structures, fascia and connective tissue and the urethra itself. This then leads to bladder leakage-- most often termed as "stress incontinence" which is leakage occurring with an increase in intraabdominal pressure.
The majority of individuals will have some degree of bladder leakage immediately after the catheter is removed. When looking further down the line, numbers are actually hard to estimate as different authors and surgeons have different ways of defining and measuring leakage. One study found that at 3 months post-prostatectomy 35% had bladder leakage. Another study found that leakage lasting more than a year happened in 11-69% of individuals. Yes, those are vastly different numbers.
How can it be treated?
As I mentioned above, leakage after prostate surgery can be so impacting for patients! And many feel guilty for being bothered by it... it's the whole, "At least I don't have cancer anymore..." guilt. But, here's the thing. Quality of life matters. Yes, not having cancer is HUGE, but YOU matter. Your life matters. And helping you live your best life? Well, that really matters a lot. So, if you're reading this and feeling frustrated about your bladder problems after surgery (or any other problems for that matter!)-- I see you. There's hope and help available!
Retraining the external urethral sphincter an be helpful for some people after prostate removal, and that's where we pelvic floor physical therapists come in. The key thing here is optimizing the muscle system, which involves retraining the pelvic floor muscles to help them be able to contract well, relax well, and coordinate. I remember working with a urologist previously who told all patients after prostatectomy to do 10 second pelvic floor contraction holds, 10 times, every hour of the day. And guess what? When I saw most of his patients, they had significant challenges with pelvic floor muscle overactivity, and some even had pelvic pain. Why? Because it was wayyyy more than THEIR pelvic floor muscles needed. The best treatment is the individualized treatment! So, if someone has pelvic floor muscle overactivity, the best treatment is the one focusing on relaxing/lengthening the pelvic floor muscles. If someone has underactivity, the goal should be in regaining strength, endurance and building control. And if a person struggles with coordination, the goal should be retraining timing and control of the pelvic floor muscles.
Research has always focused on strengthening the pelvic floor muscles, and honestly, I think this is one of the reasons we see mixed results in studies. It makes sense, and it really is what I tend to see in the clinic. I was so pleased to see this study come out a few months ago looking at an individualized pelvic floor rehab approach for patients after prostatectomy. In this study, they reviewed 136 patients who had leakage after prostatectomies, and they found that 98 of them actually had muscle overactivity with underactivity. Guess what? Only 13 had underactivity with no tension/overactivity. This is honestly what I tend to see the most clinically. In this study, they individualized treatment based on the examination findings, and they found that 89% of the patients had a reduction in their urinary leakage. 58% achieved what was deemed "optimal" improvements in their leakage. This is good news, and really highlights the benefit of having a comprehensive examination and treatment (not just going somewhere for "biofeedback training")
When a person is ready for strengthening (generally, after overactivity has been improved), the way strengthening happens actually matters. In fact, it really, really matters. Paul Hodges has done amazing research to help us better understand the continence system in men. In short, the system is different, and requires a different approach to rehabilitation. When the prostate is removed and the loss of the internal sphincter occurs, compensation must take place, and involves the external urethral sphincter, and can also include other muscles (particularly puborectalis and bulbocavernosus). So, it is very important for a clinician to evaluate the entirety of the pelvic floor muscles and not simply focus on the muscles around the anal canal. Hodges has multiple recommendations for how to be as precise as possible with pelvic floor rehabilitation, and you can read more about what he recommends here. After the right coordination, and activation of the pelvic floor muscles happens, it is so important to integrate these muscles into function. A robust home program that integrates the pelvic floor muscles into movement is key to helping a person regain bladder control!
I hope you found this information useful. I have a lot more to say about all of this, but it's late, and those thoughts will have to wait for another day! Let me know any questions you have in the comments!
~ Jessica